Greg Fredericks ND NMD Copyright 2019
Futuristic cancer therapies are now emerging from experimentation into the realm of reality. The cancer treatments that grandpa experienced was crude and simple compared to today’s multifaceted technologies. The days of highly toxic chemotherapies combined with monodimensional radiation has evolved into a wide variety of innovative futuristic treatments ranging from gene altering immunotherapeutics to nanotech based theranostics.
Immunotherapy can come in many forms, from injection of specific viruses that attack cancer in the patient, to isolating a patient’s T cells and then cultivating, re-engineering and expanding them to provide a super potent immune vaccine that is reintroduced into the patient. This provides the patient with an arsenal of specific cancer fighters. A synthetic variation called immunprophylaxis gene transfer (IGT) is also in development. In this method synthetic genes are placed in viruses which are injected into the patient. The virus then invades the DNA with its own synthetic DNA payload and creates a modified gene that instructs the cells to make powerful antibodies.
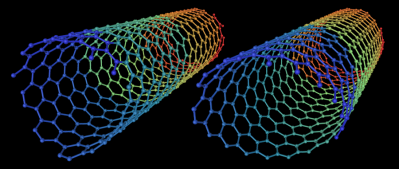 Carbon Nanotubes
Carbon Nanotubes
With nanotech based therapies, its development began more than thirty years ago but was only available on an experimental basis and to a few of the mega wealthy. Today it is becoming increasingly available to oncology patients worldwide.
Image Source: Wikimedia
Nanotech Oncology includes the use of hollow nanotubes usually made from carbon or gold although other materials are being developed. These materials are not only cytotoxic/apoptotic in themselves, acting as anticancer deterrents, but also provide a platform by which other micro amounts of chemotherapeutic agents can be piggy-backed. The synergy of these substances provides a knockout punch to tumors with minimum toxicity. These new “theranostic” treatments can give diagnostic feedback to the oncologist while providing ongoing apoptotic activity (Jain et al. 2014). The specific agents combined with nanotubes are injected around the site of a tumor for reduction before surgical removal or post-surgery to inhibit reoccurrence.
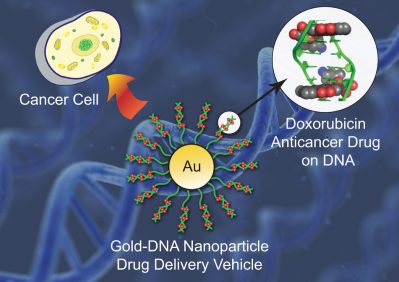
Nanoparticle Delivery System
There appears to be no limit as to what can be added to the hollow nanotubes. In one study a natural micelle form of Chitosan was combined with the chemotherapy, Paclitaxel, resulting in a novel “photothermal” apoptotic chemotherapeutic agent (Zhang et al. 2016).
The Discovery of C60
C60 are tiny three-dimensional hexagon/pentagon-shaped carbon-based nanoparticles originally called “Bucky-balls”. Early studies of Buckyballs were carried out at Rice University, Houston Texas USA in 1985. Laboratory tests on rats reported dramatic results. Rats that were given Buckyballs were claimed to live 90 times longer than normal rats. The C60 covalent nanoparticles were found to be capable of crossing the blood-brain barrier and restructuring DNA structures that determine the longevity of a cell.
Since the claims of the early findings of C60, studies have contradicted the longevity potential of the nanoparticle. One study found that because C60 has binding interactions with DNA and proteins, it causes a disturbance in the MMR pathway used for DNA repair. The authors of the study stated it might cause mutability and tumor development (Gupta et al. 2011).
What is C60’s potential?
Recent investigations have revealed that C60 reduces muscle fatigue by lowering H2O2 (hydrogen peroxide) and TBARS (thiobarbituric acid reactive substances). C60 acts as an endogenous antioxidant by increasing glutathione (GSH) and catalase (CAT) in muscles. This study found C60 is a potential therapeutic agent for reducing and correcting skeletal muscle fatigue in humans (Prylutsky et al. 2017). Another inquiry has found that C60 in olive oil significantly reduces DNA damage in cardiac and hepatic tissues in rats exposed to the mutagenic/genotoxic substance cyclophosphamide (Aly et al. 2018). These studies indicate a tissue-protective/antioxidant activity could be present in C60; however, it is premature to call it a human longevity panacea.
For what application can the C60 nanoparticle be used?
C60’s DNA binding abilities may not be a total disadvantage especially in some applications such as cancer therapy. The nanoparticle shows it can be used as an anticancer delivery platform in difficult cancers. Statistically, one of the worst types of cancer in people is liver cancer. C60 fullerenes have demonstrated apoptotic effects when combined with I-phenylanine (C60-phe) and glycine (C60 gly) against human liver cancer cells and activated by photodynamic beams. C60 has demonstrated a potential liver cancer treatment when activated by photodynamic illumination (Li et al. 2014).
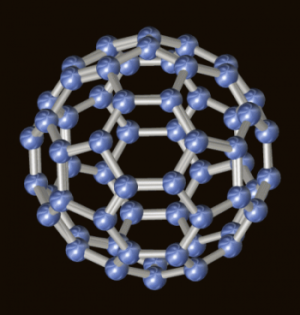
C60 Molecule
Nanoparticles similar to C60 are now being used extensively by pharmaceutical biotechnology companies in orthodox oncology (cancer) therapy. Nanoparticles of various compositions are used as a platform to piggyback microdoses of chemotherapy into tumors. K. H. Son and associates have demonstrated how carbon particles can be used as nanocarriers for a wide variety of anticancer molecular targeting drugs. These nanoparticle carriers can optimize the effectiveness of an anticancer treatment with minimal micro dosages (Son et al. 2016).

Gold Nanotubes sizzle cancer cells
Photon beams with specific infrared frequencies and sound frequencies can be used to activate the nanotubes from outside the body without additional surgical intervention (Tumish et al. 2007).
Courtesy: Jing Claussen/Ithera Medical
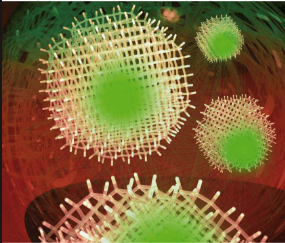
Nanoparticle Activation in Cancer
Photodynamic illumination therapy is a treatment that emits wavelengths of light from outside the body which creates an excitatory response on nanoparticles in the body. Nanoparticles of various compositions act as photosensitizing molecules that absorb the photon molecules. That is, they absorb photon light energy of specific wavelengths that generate cytotoxic reactive oxygen species (ROS) which destroy cancer cells. This could have amazing potential in inoperable and elderly applications.
This type of therapy does not produce the side effects of chemotherapy and radiation treatments and is effective on a wide range of superficial and deep-seated cancers (Sivasubramanian et al. 2019).
A new variation of Photodynamic therapy (PDT) is Sono-Photodynamic therapy (SPDT). This method uses the addition of two chlorophyll derived Sono-photo sensitizing agents along with ultrasound frequencies. The additional resonating frequencies combined with PDT, provides greater applications on difficult sarcomas and gastric adenocarcinomas. The external photo beams and sound waves create an internal resonance effect activating the nanoparticles combined with microdoses of anticancer agents to dramatically enhance cancer-killing therapy (Li et al. 2017).
Diamond patches are another form of nanotech therapy and can also be used in a similar way, placed in tissue surrounding cancer tumors. This type of treatment developed in Japan and America allows for use in situations where larger margins cannot be taken in surgical procedures. So far it has demonstrated use in oncology as well as in cardiovascular open heart surgery applications with high tolerance, in primate studies (Moore et al. 2016).
Nanodiamond Patches
Diamond nanoparticles are also used as a nano platform with chemotherapeutic drugs and for their sustained anticancer effects on their own. These are especially effective where tumors have been removed but abnormal cells may still remain. Diamond patches are installed around the margin where tumors have been extracted for greater localized anticancer defense (Gupta et al. 2017). These types of treatments have been allegedly available to the mega-wealthy for decades but are still not widely available to the general public.
Nano technology combined with CBD
Considering the research presented here, is it reasonable to postulate that C60 or other nanoparticles could provide a synergistic platform for the anticancer cannabinoid lignand anandamide? (Adinfolfi et al. 2013). Cannabinoids including CBD are highly lipophilic by nature. This chemical structure provides CBD with suitability for use with a nanotechnology delivery platform to treat a wide variety of disorders (Bruni et al. 2018).
Ancient Wisdom Rediscovered
Intriguingly, the nanotechnology being used today has similarities to anticancer treatments reaching back over 4000 years in India. Ancient Ayurvedic medicine has used a formulation known as “Ras-Rasayan” (meaning life extension) which is composed of pulverized powdered versions of diamonds, emeralds, gold, jade, rubies and mercury which has been exposed to ultra-extreme temperatures and pressure creating nanoparticles. Various mixes of these elements and precious gems were used to treat cancers of all types. The secret methods of decocting these substances were only known by a few Ayurvedic alchemists chosen to treat royalty and the wealthy. The powdered nano mercury (rendered non-toxic) is considered a precious substance in eradicating cancer according to historic Sanskrit Ayurvedic manuscripts (Puri et al. 2003). Often these particulates were mixed with black seed (Nigella sativa) oil and administered orally. These methods are crude examples of modern nanotechnology and are still in use today. The combination of nanoparticles with therapeutic herbal derivatives has been used for centuries in the ancient Indian civilization (Rege et al. 1999).
The rediscovery of ancient technology has created new refined delivery methods that can piggyback therapeutic substances such as CBD. A further activation of the nanoparticles using photon beams and sound frequencies could potentially increase the efficacy even more.
Chemotherapeutic Determination
The determining of what chemotherapeutic agent that is effective and can now be performed with far greater accuracy than ever before. The use of panels with up to 40 different chemotherapies and molecular targeting drugs are subjected to biopsy derived cancer cell samples from a cancer patient. This method is especially useful for patients with sarcomas or carcinomas of an unknown etiology. The panel spots the effective apoptotic agent without the patient being subjected to trial and error textbook treatments that could compromise QOL (quality of life). This methodology has been developed in Germany and is now widely implemented by oncology clinics throughout the world.
Oncology combines many technologies that have been around for decades but only now becoming accepted. In Germany and other countries, these treatments include sensitizing pre-treatment such as hyperbaric oxygen therapy in which additional reactive oxygen species contribute to an enhancement of chemotherapy and radiation treatments (Poff et al. 2014).
The use of hyperthermia has been determined by German and Western oncologists to dramatically affect the permeability of cell membranes of cancer cells making them susceptible to apoptosis without high dose chemotherapy. Often similar effects are also achieved with integrated medicinal herbal isolates or ozone therapy (Giustini et al. 2010). Apoptosis is the most common cell death mechanism in cancer; however other mechanisms such as autophagy, autoschizis, necrotosis, paraptosis, pyroptosis and others are being investigated for future therapy.
Using less chemo to yield greater results is the goal of a chemosensitizing method known as insulin potentiation therapy (IPT). It was first developed in the early 1980’s but was never accepted as an orthodox treatment. IPT is making a comeback as oncologists develop advances in the understanding and manipulation of insulin-like growth factor receptors (IGF) on cancer cells. Further refinement of a protocol by which less chemotherapy can yield better results and greater patient QOL is in current development (Geeraert et al. 2016).
Cryosurgery
Other futuristic approaches in oncology have led to the development of cryosurgery or freezing knife. New variations of this method continue to evolve in oncology. Currently, doctors in Beijing are experimenting with a laser-guided hollow pointed tube resembling a laparoscope containing a Freon type mixture that can freeze a tumor in seconds with minimum damage to surrounding tissue (Niu et al. 2012).
Other New Technologies
Elon Musk CEO of SpaceX and Tesla has announced (July 2019) his new creation “Neuralink”, a chip that is implanted into a person’s brain. Musk says the chip features a USB-c port which can adapt to an Apple Macbook and uses Bluetooth to connect to a small computer worn over the ear and then to a Smartphone. Neuralink can be used by stroke victims, cancer patients, quadriplegics and others wanting to enhance their memory. Up to 10 units can be inserted into a patient’s brain, which will then be connected to an iPhone app controlled by the user.
Gene Editing in Progress

The before mentioned discovery has potential to be combined with TALEN or CRISPR gene editing technology for another, as yet unexplored application. Scientists at the University of Pennsylvania have developed clinical trials using CRISPR technology as an advanced anticancer treatment. The scientists take immune cells out of 18 cancer patients, edit the cells to switch on anticancer gene mechanisms, and then infuse them back to the patient (Plumer et al. 2017). The anticancer potential of the CRISPR technology is enticing for further research grants however designer babies and production of super humans are already in progress.

Futurist and author, Juan Enriquez says that the new evolution of Homo sapiens will be “Homo evolutis”- the title of his book. Homo evolutis will be “a Hominid that takes direct control over the evolution of their species and others”.
Enriquez sees the intersection of super-advanced cellular biological and mechanical engineering giving man the ability to change his body. Enriquez predicts the adaptation of cellular regenerative mechanisms from an endangered species known as the “Axolotl” could give the future Homo evolutis the ability to regenerate limbs, organs, and brain tissue.
Naturopathic Oncologists
Integrative approaches in oncology are continuing to expand in many ways with the goal of improving patient outcomes. Naturopathic oncologists in America have emerged since 2003 and now number in the hundreds. These naturopathic medical doctors have taken additional education in the use of mainstream oncology treatments combined with knowledge in evidence-based natural therapies. By understanding the targeting of these treatments they are able to advise lifestyle, diet and exercise programs as well as orthomolecular or herbal support to reduce side effects of conventional therapies and increase QOL in patients.
Naturopathic oncologists are trained to provide assistance to orthodox oncologists and complementary support for the patient. Treatments may include correcting the terrain of the cancer patient, re-establishing circadian rhythms, immune enhancement, and other types of support for better outcomes including gut ecology. New research has found that gut ecology can play a prominent role in anticancer immune support with the discovery of new probiotic strains that play a role in antitumor activation (Daillere et al. 2016). People with cancer often have an imbalance in specific strains of gut flora (Rajagoplala et al. 2017). A recent investigation using 16srRNA amplicon sequencing of women in America with breast cancer resulted in a significant finding in their microbiota profiles. Compared to healthy women (controls), women with breast cancer had significantly elevated abundance of Bacillus Enterobacteracea, Staphylococcus Escherichia coli, and Staphylococcus Epidermidis Escherichia in their breast tissue (Urbaniak et al. 2016).
Naturopathic oncologists can play a prominent role in the rebalancing of an oncology patient’s microbiota and prevention of potential degenerative conditions.
Cymatics and the Cymascope
Cymatics is the science of how sound is made visible. Audio frequencies subjected to a medium such as water create a visual vibrational pattern that is unique to that medium. In an oncology application this methodology has been utilized to differentiate between normal cells and cancerous tissue.
Originally described as the science of sonocytology, this technology was discovered by Dr. James Gimzewski in 2002. Gimzewski found that each cell generates its own unique kind of “song” depending on its structure. In an article published in Advances in Intelligent Systems and Computing from April 2021, associate Professor Sung Chul Ji and Professor Beum Jun Park of Rutgers University in collaboration with John Stuart Reid are credited for putting together the first novel classification methodology for use in surgical oncology.
The first acoustic scientific instrument known as the Cymascope has been in use since 2021 and has demonstrated its ability to differentiate between normal cells and abnormal tissue. This enables surgeons to better determine margins of tissue removal more accurately when performing tumor extraction.
The Cymascope functions by transforming sonic periodicities (sound forms) into water wavelet periodicities (visible forms) making the cancer cells visible by sound. The Cymascope uses fused quartz crystal to provide optimal results due to its ability to reveal resonating imperfections at a microscopic level creating an analogue of sound. “When sound is injected into water it first appears in epicenter of the cuvette, then it moves to the circular boundary where it reflects back. If those reflections incur imperfections then the accuracy of the model would be compromised – which is why we use quartz” -according to Reid.
Natural resonances are tuned out in order to create a flat frequency response. This enables an accurate detection of an abnormal vibrational pattern particular to cancer cells.
Special eyewear is used by the surgeon that enables them to see cellular tissue that is scanned by a Ramen stereoscope lased. The eyewear provides a cymatic picture making it easier to detect the cancerous cells from the normal tissue. The Cymascope technology is an exciting new advancement for future oncology with no risk for patients.
New orthodox technologies combined with evidence-based natural therapies create an exciting new realm of possibilities for cancer patients unlike anything before.
